- Home
- »
- Glossary Of Terms
- »
- 1095 C Form
Form 1095-C: Employer-Provided Health Insurance Offer and Coverage
IRS Form 1095-C is a tax document required under the Affordable Care Act (ACA). It reports the health insurance coverage that large employers (those with 50 or more full-time employees) offered to their workforce. Employees typically receive it early in the year, usually by January 31, along with their W-2 and other tax forms.
The form provides details about:
- Whether your employer offered you health coverage during the year.
- Which months you and your dependents were eligible for employer-sponsored coverage.
- The cost of the lowest-priced monthly premium for self-only coverage.
Purpose: The IRS uses Form 1095-C to ensure that employers comply with ACA employer mandates and to confirm that individuals had access to qualifying health coverage. Even though the federal penalty for not having insurance was eliminated in 2019, some states (like California, Massachusetts, and New Jersey) still require proof of coverage for tax purposes.
Key point: Receiving a 1095-C does not mean you owe taxes. It is an informational form that helps you complete your tax return accurately and confirm your eligibility for potential tax credits.
Who Receives Form 1095-C?
If you were a full-time employee at a company with 50 or more employees, you should receive a 1095-C—even if you declined coverage or had insurance through another source (like a spouse’s plan or Medicare). Self-insured employers also report actual months of coverage on this form.
How to Use Form 1095-C
- Keep it with your tax documents—similar to your W-2.
- You do not need to attach it to your tax return, but you may need the information when filing with tax software.
- If you received health coverage through the Marketplace (Obamacare), you will instead use Form 1095-A.
Example: An employee at a company with 200 staff members receives a 1095-C showing that health insurance was offered all 12 months of 2023. Even if the employee declined the coverage, the IRS will have a record that the employer met ACA requirements.
1095-A vs 1095-B vs 1095-C (Quick Comparison)
All three are Affordable Care Act (ACA) forms, but each serves a different purpose and comes from a different issuer. Use this guide to know which one applies to you and how to use it at tax time.
Form 1095-A — Health Insurance Marketplace Statement
- Who receives it: Individuals and families who enrolled in coverage through a federal or state Marketplace.
- Issuer: The Marketplace (Healthcare.gov or your state exchange).
- What it reports: Monthly premiums, advance premium tax credit (APTC) paid to your insurer, and months of coverage.
- How it’s used: You must use 1095-A to complete Form 8962 to reconcile the premium tax credit on your tax return.
- Example: You bought a silver plan on Healthcare.gov with APTC—your 1095-A shows what was paid so you can reconcile credits.
Form 1095-B — Health Coverage
- Who receives it: Individuals covered by government programs (Medicaid/Medicare), small-group employer plans, or other non-Marketplace coverage.
- Issuer: Your insurance provider or a government program.
- What it reports: Months you had minimum essential coverage.
- How it’s used: Keep it for your records; you typically do not attach it to your federal return.
- Example: You had coverage through a small employer’s insurer—1095-B confirms your covered months.
Form 1095-C — Employer-Provided Health Insurance Offer and Coverage
- Who receives it: Full-time employees of Applicable Large Employers (generally 50+ full-time employees), whether they accepted or declined the offer.
- Issuer: Your employer (and 1094-C transmittal goes to the IRS).
- What it reports: Whether coverage was offered, affordability information, and (for self-insured employers) months actually covered.
- How it’s used: Keep for records or enter details in your tax software if prompted; typically not attached to your federal return.
- Example: Your large employer offered coverage all year—1095-C documents the offer and your eligibility.
Which form do I use on my taxes?
- Marketplace coverage: Use 1095-A to complete Form 8962 (required for reconciling premium tax credits).
- Employer or other non-Marketplace coverage: Keep 1095-B and/or 1095-C for your files; you usually don’t attach them to your federal return.
- State mandates: Some states require proof of coverage—keep your 1095 forms in case your state return asks for details.
Key differences at a glance
- 1095-A: Marketplace-specific; ties directly to the Premium Tax Credit.
- 1095-B: Confirms coverage months from an insurer or government program.
- 1095-C: Documents an employer’s offer of coverage (and coverage months if self-insured).
Tip: If you got coverage from more than one source in a year, you may receive multiple forms. Keep them all together with your W-2 and other tax documents.

FAQs 1095 C Form
You don’t need to attach it to your tax return, but you should keep it for your records and may need it when filing.
No. It’s an informational form only and does not affect how much tax you owe.
To document employer-provided health insurance offers and help the IRS enforce ACA requirements.
Because your employer was required to report that they offered you coverage, even if you declined.
Other Free Resources
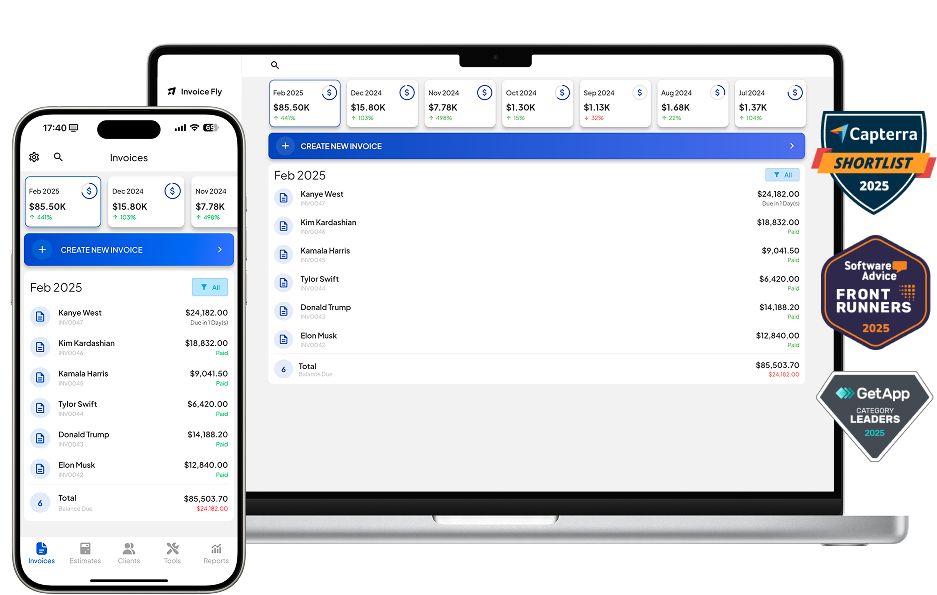
Try Invoice Fly Today
- Send quotes & invoices in seconds
- Collect card & online payments
- Receive instant notifications
- Win more jobs